The 2-in-1 surgery includes a major surgery and a "super procedure", with high complexity, requiring smooth coordination between 2 surgical teams and the anesthesia and resuscitation team.
Giant hernia and large gallstones causing biliary obstruction
Traveling hundreds of kilometers from Cambodia to Ho Chi Minh City, Ms. MC (65 years old) was admitted to Gia An 115 Hospital in an emergency with chest pain - right flank. The patient's relatives said that in the previous 2 months, she had repeatedly had dull pain in the right flank accompanied by chest pain. In the 3 days before being admitted to the hospital, the pain gradually increased, accompanied by a low fever of 38 degrees Celsius and nausea, making the family decide to take her to Vietnam for treatment.

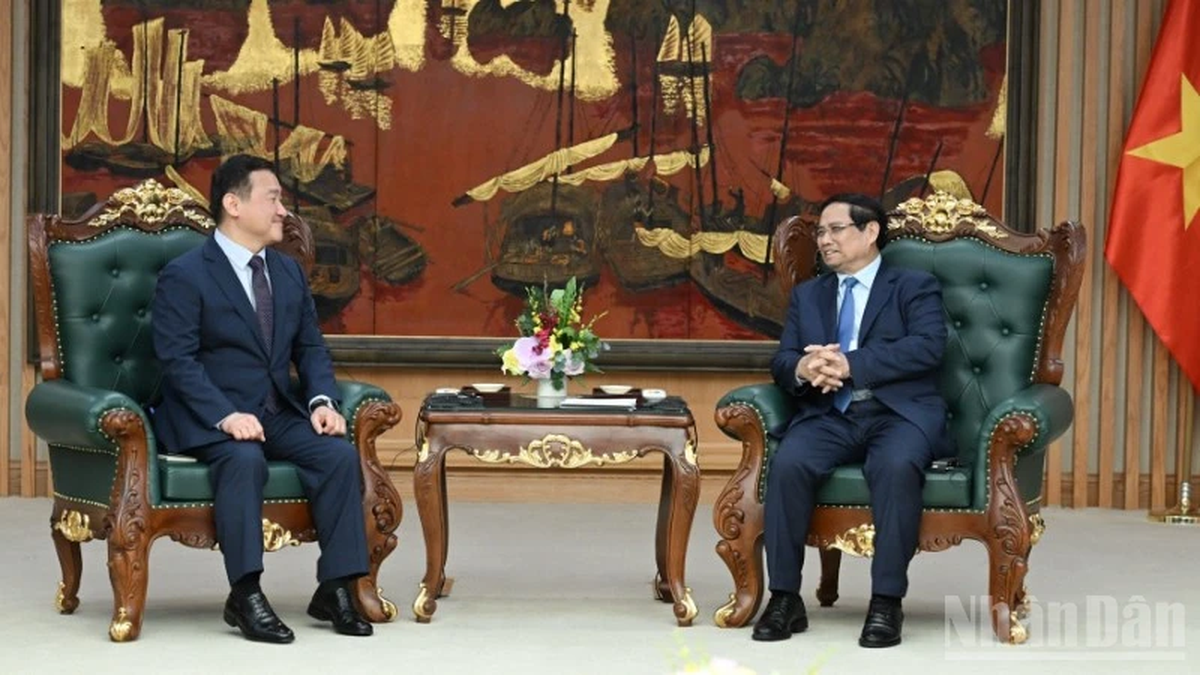
Master - Doctor Nguyen The Toan performs surgery on a patient
Photo: BVCC
At Gia An 115 Hospital, examination and imaging results showed that the patient had two serious abdominal diseases at the same time.
The first is a giant abdominal wall hernia in the left iliac region measuring 29x18 cm. The hernia sac contains almost all the loops of small intestine, left colon, mesentery and omentum - potentially leading to intestinal torsion leading to intestinal obstruction - intestinal necrosis, abdominal infection, peritonitis if not treated promptly.
The second is a 12x15 mm stone at the end of the common bile duct, the common bile duct is dilated 12 mm (horizontally). The large stone causes bile obstruction and biliary tract infection.
“Normally, with these two diseases, the patient will have to undergo two separate surgeries - one to treat the abdominal wall hernia, one to treat the common bile duct stones. However, in this case, in addition to professional factors, doctors also have to face an “invisible challenge” - the patient's fear of surgery,” said pancreatic biliary specialist, master - doctor Nguyen The Toan, Head of Surgery Department, Gia An 115 Hospital.
Previously, Ms. MC had to stay in intensive care for 4 months after abdominal aortic bypass surgery in Thailand - a haunting experience that made her especially afraid of surgery. Therefore, doctors had to carefully consider the professional aspect to choose the optimal intervention plan, minimizing the number of invasive procedures while ensuring the highest treatment efficiency.
However, combining a major surgery and a "super procedure" under the same anesthesia is a big challenge for the entire team, especially when the patient has many high-risk underlying diseases such as high blood pressure, type 2 diabetes, chronic kidney disease and obesity.
One anesthesia - 2 "rescues"
The special surgery was performed with close coordination between two surgical teams and anesthesia and resuscitation, in a single anesthesia session.
The first team performed surgery to treat abdominal wall hernia. The patient was placed on the right side at a 60-degree angle to optimally access the left hernia area. The surgeons separated each layer, released the hernia sac, returned the entire herniated organ to the abdominal cavity, and restored the abdominal wall with an anti-adhesive artificial mesh, helping to reinforce it firmly while limiting the risk of intestinal adhesions after surgery.
Immediately afterwards, the second team performed endoscopic retrograde cholangiopancreatography (ERCP), performed sphincterotomy, and successfully removed a large stone from the distal end of the common bile duct - completing the dual intervention under the same anesthesia.
After surgery, the patient recovered well and was discharged in stable condition.

Patient recovers after surgery
Photo: BVC
Symptoms of abdominal wall hernia, bile duct stones
According to Master - Doctor Nguyen The Toan, abdominal wall hernia is a disease that occurs due to the displacement of organs from the abdominal cavity to the abdominal wall through a weak position on the abdominal wall. The disease can be congenital or acquired. Acquired abdominal wall hernia is common in people with a history of abdominal surgery, or after abdominal trauma, and can also be caused by prolonged increased abdominal pressure (obesity, chronic cough, constipation). Weak abdominal wall, surgical site infection, or malnutrition increase the risk.
Symptoms are an abnormal bulge in the abdominal wall that grows larger when coughing, straining, standing for a long time, and shrinks when lying down. The disease is treated with laparoscopic surgery (for small hernias) or open surgery (for large hernias). If not treated promptly, it can cause intestinal obstruction, intestinal necrosis, peritonitis, and be life-threatening. People who have had surgery, abdominal trauma, or have risk factors such as obesity or chronic cough should see a doctor immediately if they notice an abnormal bulge in the abdomen.
Regarding common bile duct stones, Dr. Toan warns that if not treated promptly, stones can cause bile duct obstruction - liver failure, sepsis or acute pancreatitis. Warning signs that require immediate medical attention include: Pain in the right hypochondrium (especially after a fatty meal), fever, nausea, possibly accompanied by jaundice, dark urine due to bile duct obstruction. If the pain persists with fever, the patient should go to a medical facility immediately for timely treatment.
Source: https://thanhnien.vn/mot-lan-gay-me-2-can-thiep-lon-thoat-vi-thanh-bung-va-soi-tac-mat-185250705173952792.htm


![[Photo] Brilliant red of the exhibition 95 years of the Party Flag lighting the way before the opening](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/27/e19d957d17f649648ca14ce6cc4d8dd4)


![[Photo] Prime Minister Pham Minh Chinh receives CEO of Samsung Electronics](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/26/373f5db99f704e6eb1321c787485c3c2)
![[Photo] Prime Minister Pham Minh Chinh chairs meeting of National Steering Committee on International Integration](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/26/9d34a506f9fb42ac90a48179fc89abb3)



























![[Photo] General Secretary To Lam attends Meeting with generations of National Assembly deputies](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/8/27/d869c6b3e4da42399e2cd0f4ca26050c)






























































Comment (0)