From personalized vaccines and next-generation immunotherapies to powerful support from artificial intelligence and biotechnology, modern medicine is closer than ever to the goal of turning cancer into a disease that can be controlled long-term, and even completely cured in some cases.
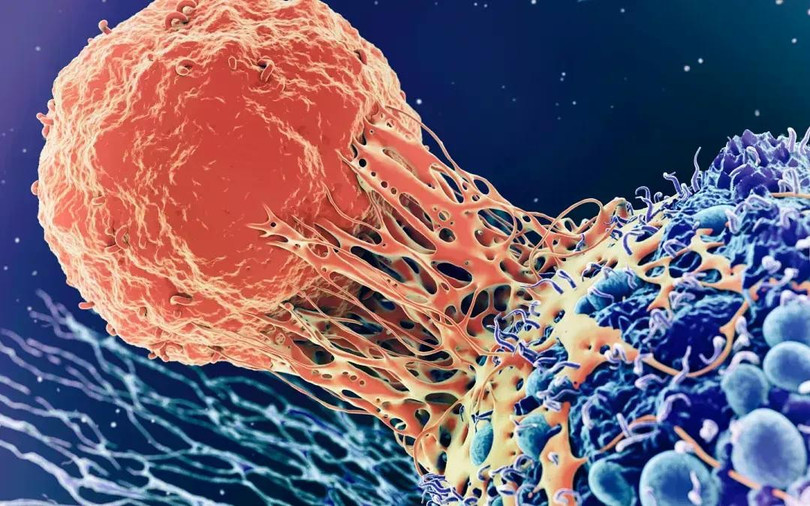
Breakthrough in cancer treatment by 2025
One of the most revolutionary achievements since the beginning of 2025 is the development and application of personalized cancer vaccines - vaccines designed specifically for each patient, based on analysis of the genome and biological characteristics of the tumor.
In the US, a clinical trial involving the Dana-Farber Cancer Institute and the Yale Cancer Center has produced stunning results: Nine patients with advanced kidney cancer have gone into complete remission after three years of treatment with a personalized vaccine, with no signs of recurrence to date. Scientists say the vaccine works by training the immune system to recognize and destroy cancer cells based on the tumor’s unique genetic makeup—a step forward from traditional immunotherapy approaches.
In Europe, a personalized mRNA vaccine trial is underway in more than 30 hospitals in the UK, Germany, Belgium, Spain and Sweden, with the trial scheduled to be completed in 2027. Health experts expect that if the vaccine delivers similar results as in the US, it will become one of the mainstays of cancer treatment in the next decade.
The second, equally groundbreaking achievement is immunotherapy, which is expanding its scope and increasing its effectiveness in cancer treatment. In recent years, immunotherapy has become a mainstay in cancer treatment, and 2025 continues to see impressive progress. A study at Memorial Sloan Kettering Cancer Center (USA) published earlier this year showed that the immunotherapy drug dostarlimab, a member of the immune checkpoint inhibitor group, helped 80% of cancer patients with MMRd (Mismatch Repair Deficiency) mutations achieve complete remission, without surgery or chemotherapy.
This result is particularly notable in the treatment of difficult cancers, such as colorectal, esophageal, gastric and prostate cancers - diseases that often require invasive surgical intervention. The use of dostarlimab helps the immune system recognize cancer cells as "foreign" and destroy them precisely, minimizing damage to healthy tissue.
In addition, a new generation of immunotherapies is also being widely researched, including: Bispecific antibodies (capable of attaching to cancer cells and immune cells at the same time, creating a bridge to increase the effectiveness of destroying diseased cells); CAR-T and CAR-NK cell therapy (Designed to reprogram the patient's immune cells to attack cancer more actively and strongly. This year, several clinical trials have shown positive results in brain and pancreatic cancers - the two types with the worst prognosis today).
Personalized treatment down to the cell level
The explosion of artificial intelligence (AI) is opening a new chapter in cancer treatment. Modern machine learning systems are capable of processing large amounts of biomedical data from gene sequencing, diagnostic imaging results, and medical records to create personalized treatment regimens, predict drug response, and determine the risk of recurrence.
In India, AI has been deployed to aid in early detection of breast and lung cancer in rural areas lacking specialist doctors. This has significantly increased the rate of early cancer detection, improving prognosis and treatment costs.
One of the standout studies this year comes from the Mayo Clinic, where scientists are using AI to analyze the gut microbiome, which has been shown to play a key role in regulating immune responses and treatment outcomes. Understanding the interactions between microbes and medications can help doctors design diets, add probiotics, or modify treatment regimens to reduce side effects and improve treatment outcomes.
Biotechnology: Precise intervention at the cellular level
Along with AI, biotechnology is also playing an indispensable role in the cancer treatment revolution. One of the advanced methods being deployed is bioelectric therapy, which uses low-frequency electric fields to inhibit the division of cancer cells.
Novocure (USA) has developed the Tumor Treating Fields (TTFields) device, which works by emitting electromagnetic waves that disrupt the DNA replication process in cancer cells. This device is used in conjunction with chemotherapy, and is especially effective in treating brain tumors and mesothelioma - two diseases with low survival rates.
In addition, gene therapy continues to see breakthrough applications. CRISPR gene editing technology is being tested to “turn off” cancer-causing mutated genes or reprogram immune cells. In India, AIIMS Hospital has successfully applied gamma knife technique - a form of non-invasive surgery using highly precise radiation - to treat retinoblastoma in children, helping to preserve vision and limit damage to healthy tissue.
According to the World Health Organization (WHO), global cancer cases are expected to increase by 77% by 2050, reaching more than 35 million cases per year. Against this backdrop, the medical advances of 2025 send a powerful message: Cancer is no longer a death sentence.
Treatment strategies are shifting from a “one size fits all” approach to deep personalization – where each patient is treated based on their unique genetics, immune system, living environment and microbiome. High technology is no longer a fantasy but has become an essential tool to support doctors in every step of treatment from diagnosis, treatment regimen, monitoring to relapse prevention.
The future of cancer treatment is not just about cure, but about managing cancer as a manageable chronic disease, improving quality of life, extending life expectancy and bringing hope back to millions of families around the world.
It is impossible not to mention the wave of new cancer drugs being approved, significantly expanding the options for patients:
Ivonescimab: The first bispecific antibody that inhibits both PD-1 (an immune checkpoint) and VEGF (vascular endothelial growth factor), attacking cancer on two fronts. It has been approved in China and is in phase III in the US for non-small cell lung cancer.
Repotrectinib (trade name: Augtyro): A new generation tyrosine kinase inhibitor, approved by the US Food and Drug Administration (FDA) for the treatment of non-small cell lung cancer with ROS1 mutations - a rare but difficult-to-treat mutation.
Penpulimab: A PD-1 antibody approved by the FDA in April 2025, it is particularly effective in treating recurrent or metastatic non-keratinizing nasopharyngeal cancer - a common form of cancer in Asia. These drugs not only improve treatment efficacy but can also be flexibly combined with immunotherapies and chemotherapy, creating a more comprehensive treatment strategy for patients.
Source: https://baohatinh.vn/nhung-buoc-tien-moi-trong-dieu-tri-benh-ung-thu-post289493.html






























































































Comment (0)